Inhalers vs. Nebulizers for COPD: How They Work, When to Use Each, and Safety Tips
Outline and What You’ll Learn
Before diving into valves, particles, and cleaning routines, it helps to know the map. This article opens with a guided outline so you can scan what’s ahead and jump to the part that answers your immediate question. The topic matters because inhaled therapy is the foundation of symptom relief and flare-up prevention in chronic obstructive pulmonary disease, yet confusion about devices is common. Many people are handed a device at discharge and told to “use as directed,” only to find that technique, timing, and maintenance make or break results. Below is the roadmap, followed by expanded sections with practical detail and examples you can apply today.
Section 1 – The science of delivery: how inhalers and nebulizers move medicine from canister or chamber into your lungs, why particle size matters, and how breathing patterns influence where the dose lands.
Section 2 – Effectiveness and convenience: what studies suggest about outcomes when devices are used correctly, how inspiratory flow, dexterity, time, portability, and cost shape real-life choices, and which situations tilt the decision one way or the other.
Section 3 – Technique and safety: step-by-step instructions for common inhaler types and nebulizers, plus maintenance routines that keep microbes out and medication potency in, with side effect checks and warning signs that deserve attention.
Section 4 – Putting it all together: everyday scenarios such as morning routines, travel days, smoky air, or a sudden flare; how to build a simple action plan with your care team so you know when to switch devices, when to escalate, and when to seek urgent help.
Section 5 – Conclusion and takeaways: a concise wrap-up that ties science to habits, offers decision prompts you can keep on your fridge, and encourages periodic “device checkups” to keep your therapy aligned with your goals.
Use this outline like a trail guide. If you prefer to skim, look for the short bullet-style cues inside paragraphs. They highlight device selection rules of thumb, technique reminders, and quick safety checks you can apply immediately:
– Start with the device you can use correctly every time.
– Match delivery to your breath: lower flow often favors nebulization.
– Clean gear on a schedule, not only when it looks dirty.
– Track symptoms and adapt with your clinician’s input.
The Science of Delivery: How Inhalers and Nebulizers Work
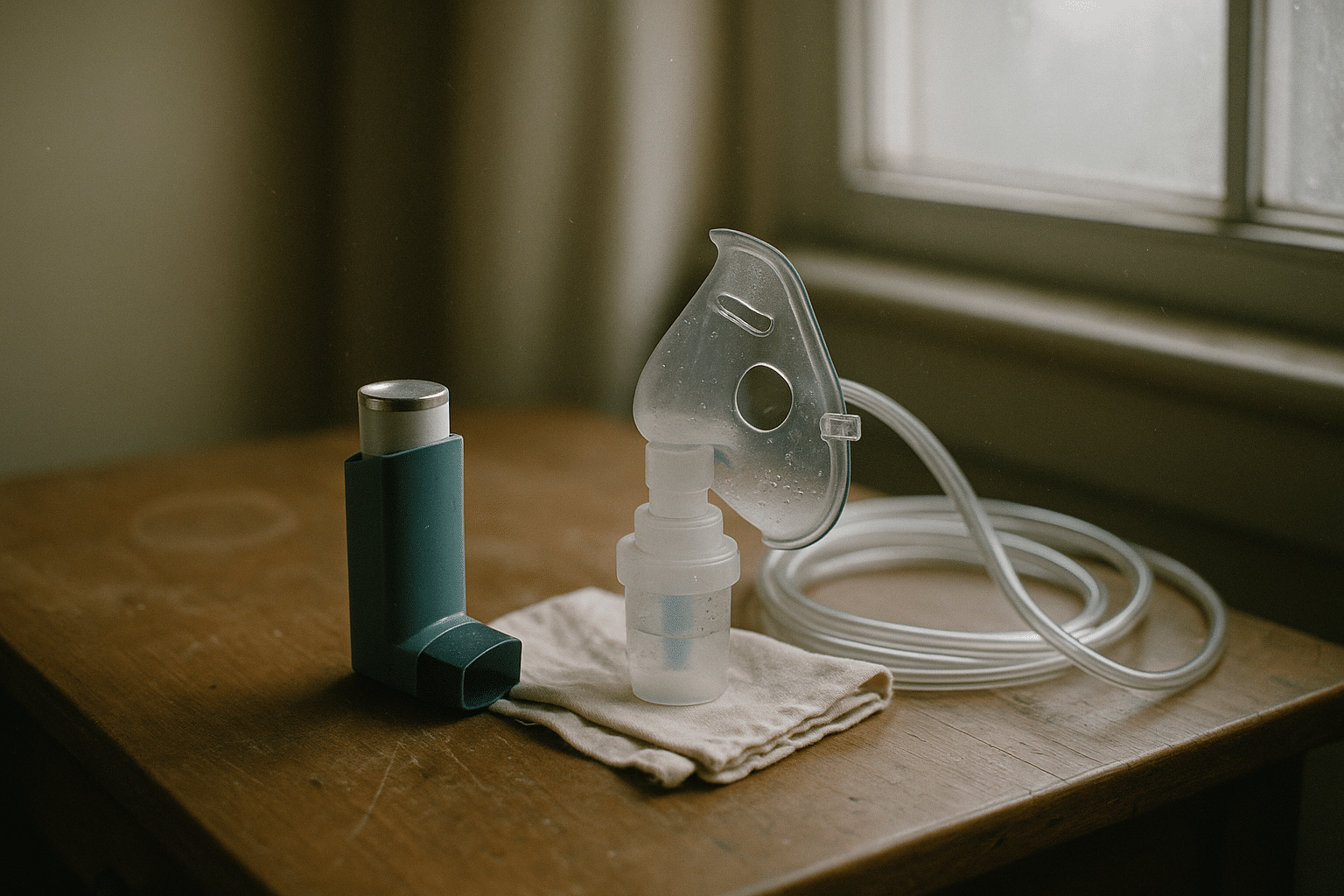
Inhaled therapy hinges on a simple goal: carry medicine deep into the airways while wasting as little as possible in the mouth and throat. Two families of tools do this work. Handheld inhalers package medication in compact devices you can slip into a pocket, while nebulizers turn liquid medicines into a fine mist you inhale over several minutes. The difference is more than form factor; each route relies on a different physics story, and that story determines how well the dose reaches the lungs.
Pressurized metered-dose inhalers release a measured spray the moment you press the canister. The aerosol contains tiny particles, many in the sweet spot of roughly 1 to 5 micrometers, which is small enough to slip past the throat yet large enough to avoid being breathed straight back out. Success depends on timing a slow, steady breath to match the puff. Dry powder inhalers load a powder that you pull into motion with your own breath; they typically work best when you can generate a brisk inhalation. Soft-mist inhalers deliver a slower-moving cloud that lingers a bit longer, which can be helpful if coordination is tricky. Across these designs, one principle repeats: inhalation flow and technique decide the fraction of medicine that reaches the lungs.
Nebulizers, by contrast, aerosolize a liquid dose over a span of about 5 to 10 minutes. Jet systems use compressed air to shatter droplets, while mesh systems vibrate a fine screen to create a consistent mist. Because the mist is delivered continuously, you simply breathe normally through a mouthpiece or mask. That makes nebulization less dependent on perfect timing, which can be a relief during a flare when every breath feels like work. In laboratory settings, both inhalers and nebulizers can produce efficient lung deposition; in real life, the winner is the device you can use correctly and consistently.
Three practical physics notes anchor this picture:
– Particles roughly 1–5 micrometers tend to reach the lower airways.
– Rapid, forceful inhalations pull powders effectively but can slam sprays into the throat.
– Slow, steady breaths reduce turbulence and improve deep delivery.
Put differently, inhalers are like sprint relays—precise and quick—while nebulizers are like slow, even jogs that get you to the same destination with fewer coordination demands. Knowing your breathing pattern and comfort with device steps is the first clue for choosing between them.
Effectiveness, Convenience, and Choosing What Fits You
Do inhalers or nebulizers work “better” for COPD? When used correctly, large comparative studies and international guidelines generally find similar clinical outcomes for day-to-day symptom control and prevention of exacerbations. The catch is in those two words—used correctly. Real-world research repeatedly shows that a high share of users make technique errors with handheld inhalers, from mistimed puffs to breaths that are too fast or too shallow. Error rates in some surveys have exceeded half of users. Nebulizers sidestep timing issues, but they ask for time, power, and cleaning discipline. In practice, the right tool is the one you can operate accurately, day after day, in your real life.
Consider these decision factors when weighing options:
– Inspiratory flow: Dry powder devices often need a brisk inhale; if your breath is limited during a flare, nebulization can be more forgiving.
– Coordination: Press-and-breathe timing challenges can be eased by add-on chambers for sprays, but some people still prefer the “just breathe” simplicity of a nebulizer.
– Time and setting: A handheld dose takes seconds; nebulization typically takes several minutes. Mornings on the go may favor inhalers; evenings at home may welcome a calm nebulizer session.
– Portability and power: Inhalers slip into pockets; nebulizers may need an outlet or charged battery.
– Cost and supplies: Inhalers bundle medicine and device; nebulizers require solutions, cups, tubing, and periodic part replacement.
Data points can help frame expectations. Typical nebulizer sessions last about 5–10 minutes per medication. Lung deposition with pressurized sprays varies widely with technique; studies suggest around a tenth to a few tenths of the dose may reach the lungs, often higher with a holding chamber and proper pacing. Dry powders can be highly efficient at adequate flow rates, but performance drops if the breath is weak. These are ranges, not promises, and they reinforce a practical rule: choose the device whose requirements you can meet consistently, even on bad days.
Scenarios illustrate the trade-offs. Someone with strong, steady breath and a busy schedule may rely on a handheld device for daily therapy and reserve nebulization for rough patches. Another person with arthritis or cognitive load may prefer nebulization’s simplicity despite the time cost. During smoky air or respiratory infections, when breathing feels tighter, even an inhaler-first person might temporarily shift to nebulized bronchodilators because normal breathing is all that’s required. The device can follow the day, not the other way around.
Technique, Maintenance, and Safety Essentials
Correct technique transforms good medicine into good outcomes. For pressurized spray inhalers, shake if directed, exhale gently, start a slow inhale, press at the very start of the breath, and keep drawing for a full, steady lungful. Hold your breath briefly—five to ten seconds if comfortable—then exhale. If a second puff is prescribed, wait about half a minute and repeat. For dry powders, load the dose, exhale away from the mouthpiece, seal your lips, inhale sharply and deeply, hold briefly, then exhale. For soft-mist designs, prepare the device per instructions, inhale slowly and steadily through the released cloud, and hold briefly. A breath-holding pause increases the time particles have to settle where they are needed.
Nebulizer technique is straightforward: place the measured dose in the cup, sit upright, breathe normally through the mouthpiece or a well-fitted mask, and continue until sputtering indicates the chamber is nearly empty. Gentle diaphragmatic breaths can improve comfort. Tapping the side of the cup intermittently helps collect residual droplets. After use, disassemble and clean the parts that contact medication and your breath.
Maintenance protects both lungs and equipment:
– Daily after use: Wash the cup, mouthpiece, and mask in warm, soapy water, rinse well, and air-dry on a clean towel.
– Several times a week: Disinfect per manufacturer guidance, such as with a suitable solution or heat method if approved.
– Regularly: Replace filters and worn tubing as recommended; check for cracks, cloudy plastic, or warped parts that affect performance.
– For inhalers: Wipe mouthpieces to prevent residue; keep caps on; track doses if the device includes a counter or keep a simple log.
Safety tips anchor every routine:
– Do not share devices or mouthpieces.
– Rinse your mouth after inhaled corticosteroid use to reduce the chance of thrush.
– Monitor for side effects such as tremor, palpitations, dry mouth, hoarseness, or cough; report persistent or severe symptoms.
– Avoid doubling doses after a missed dose unless explicitly told to do so by your clinician.
– If symptoms escalate—rising breathlessness, worsening cough, bluish lips, drowsiness, or readings on a home oximeter dropping below your target range—follow your action plan and seek urgent care.
Finally, store medications and devices away from heat and humidity, and keep a small “go kit” ready for travel: your primary inhaler, a rescue option if prescribed, spacer or holding chamber if used, and neatly bagged nebulizer parts with a clean backup cup. Good habits are the quiet engine of safe, effective therapy.
Conclusion and Actionable Takeaways for People Living with COPD
Inhalers and nebulizers are different routes to the same destination: delivering medicine to the airways where it can relax muscles, quiet inflammation, and clear the path for easier breaths. In controlled settings they can be equally effective; in everyday life, the device you can use accurately and consistently is the one that will likely serve you well. Let your choice flex with your day and your breathing, not with rules set in stone. A light, portable inhaler might carry your mornings; a calm, unhurried nebulizer session might suit evenings or flare days. Both have a home in a thoughtful plan.
Build a simple action plan with your care team and post it where you can see it. Include three parts:
– Green zone: your daily maintenance device and dose, technique reminders, and activity targets.
– Yellow zone: signs of a flare, when to add or switch to nebulization, and how long to try before reassessing.
– Red zone: danger signs that trigger immediate care, transport arrangements, and phone numbers.
Pair the plan with periodic device “checkups.” At each appointment, ask for a quick technique review—ten minutes of coaching can pay off for months. Confirm that your inspiratory flow, grip strength, and daily routine still match your chosen device. If something has changed—new arthritis, a flare that leaves you winded, or a schedule that’s tightened—adjust the plan. Many people benefit from keeping both options available: a familiar inhaler for routine days and a ready-to-go nebulizer for tougher ones. The goal isn’t loyalty to a tool; it’s reliable delivery of medicine to the small airways, day after day.
Above all, give yourself credit. Learning device steps, cleaning parts, and noticing early warning signs are practical skills, not character tests. With steady technique, regular maintenance, and a plan that meets you where you are, inhalers and nebulizers become partners in a life shaped more by your choices than by your symptoms.


