Comprehensive Guide on How To Relieve A Stuffy Nose
Outline:
– Why noses get congested and why it can feel worse at night
– Home techniques: saline irrigation, steam, humidifiers, hydration, and positioning
– Pharmacy choices: nasal steroids, antihistamines, decongestants, and safe use
– Environment and habits: allergens, humidity, air quality, and daily routines
– When to seek care, prevention strategies, and a practical wrap‑up
Introduction:
Most people will battle a stuffy nose several times a year, whether from a cold, seasonal triggers, or indoor irritants. Nasal congestion reduces sleep quality, dulls concentration, and can even raise the risk of sinus pressure headaches. The good news: relief is often within reach using a mix of simple home measures and informed choices. The sections below translate medical know‑how into steps you can apply today, with clear notes on safety and when to get personalized help.
What Actually Causes a Stuffy Nose (and Why It Feels Worse at Night)
A “stuffy nose” is less about too much mucus and more about swollen nasal tissues. The inside of your nose is lined with delicate blood vessels and spongy structures called turbinates. When these blood vessels widen and the lining becomes inflamed—because of viruses, allergens, irritants, or temperature shifts—the passageway narrows. Think of it like a busy tunnel during rush hour: even normal traffic (air) slows to a crawl when a lane is closed. This swelling traps mucus, disrupts the tiny cilia that sweep debris along, and leaves you feeling both blocked and drippy.
Common drivers include short‑lived viral infections, seasonal or perennial allergies, nonallergic rhinitis triggered by scents or smoke, and structural factors like a deviated septum or enlarged turbinates. Hormonal shifts (including during pregnancy), certain medications, and temperature or humidity swings can also tip the balance toward congestion. In colds, the first 48–72 hours often bring the heaviest inflammation; in allergies, repeated exposure keeps the lining on high alert. Over time, persistent inflammation can sensitize the nose, making once‑minor irritants feel like major obstacles.
Nighttime often exaggerates the problem. Lying flat increases blood flow to nasal tissues, gravity redistributes fluids, and one side may clog more depending on how you sleep due to the normal nasal cycle (alternating congestion from one nostril to the other). Dry bedroom air thickens mucus, making it harder for cilia to move it along. Even reflux that creeps up at night can irritate the upper airway and add to morning stuffiness. Two practical implications follow: small changes in position and humidity can noticeably alter how open your nose feels, and your “worst side” at bedtime may switch by morning simply because of natural cycling—not because your cold suddenly got worse.
Home Techniques You Can Try Today: Saline, Steam, and Simple Physics
Before reaching for a box from the pharmacy shelf, start with gentle, well‑studied basics. Saline irrigation rinses away allergens, thick secretions, and irritants, while helping the cilia beat more effectively. Isotonic saline (about 0.9% salt) is comfortable for regular use; hypertonic solutions (around 2–3%) may reduce swelling a bit more for some people but can sting. Rinsing once or twice daily during congestion can improve symptoms and, in many cases, reduce the need for other medications.
Technique matters. Use sterile or distilled water, or water that has been boiled for at least one minute and cooled, to prepare or dilute saline. Lean over a sink, tilt your head slightly forward and to the side, and let gravity carry the rinse through one nostril and out the other; repeat on the opposite side. Device choice—squeeze bottle, neti‑style pot, or bulb syringe—comes down to comfort and control. Clean and air‑dry your device after each use to keep it hygienic.
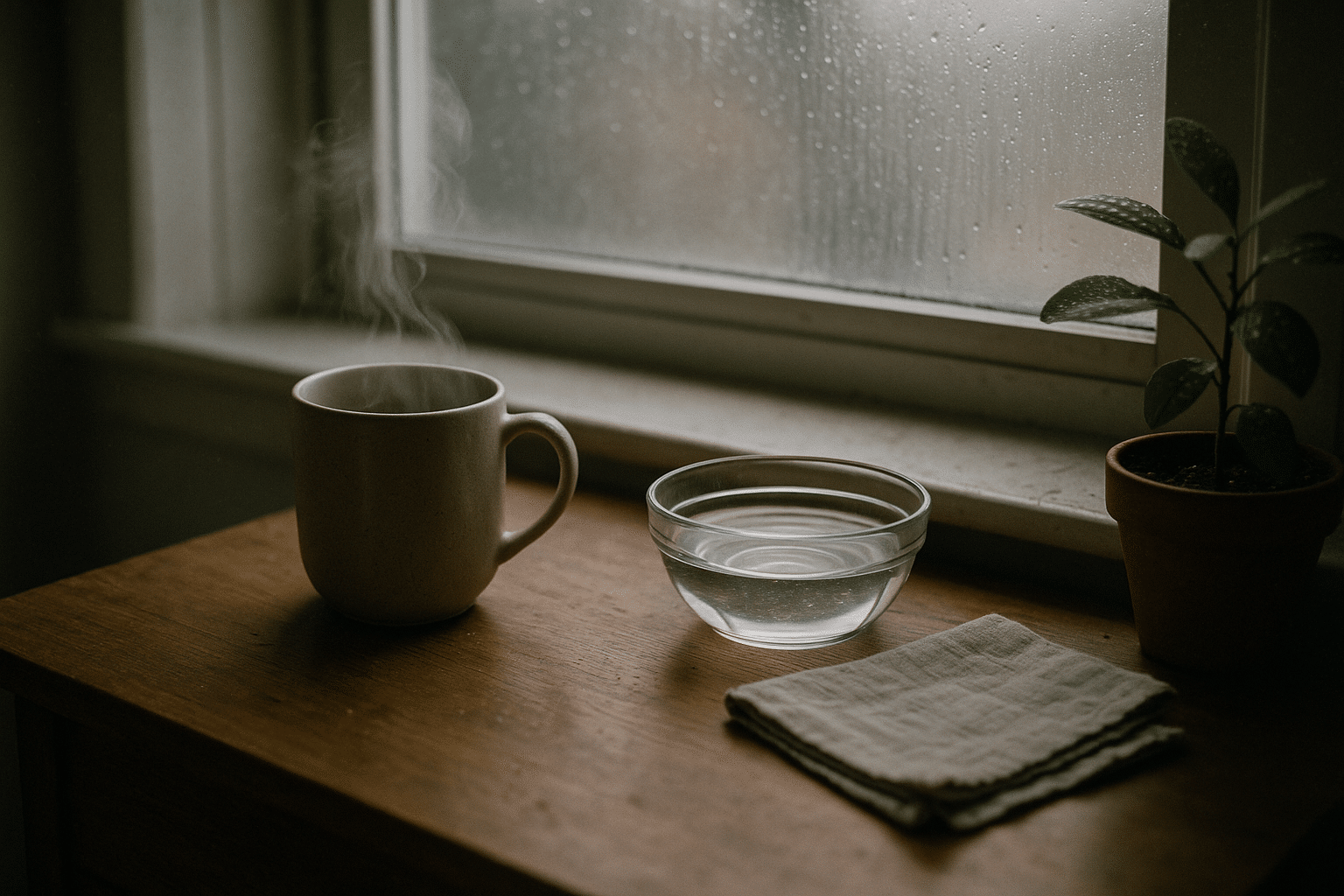
Steam can temporarily soothe irritated tissues and loosen thick mucus. A warm shower, a bowl of hot water with your face held at a safe distance, or simply inhaling warm mist helps many people feel more open, even if the effect is short‑lived. A room humidifier set to moderate humidity (roughly 40–50%) adds moisture to the air; too much humidity can promote mold, so aim for the middle. Staying well hydrated thins secretions; warm teas or broths are as much about comfort as chemistry, but the fluid counts. A warm compress across the cheeks and bridge of the nose can ease pressure by encouraging drainage.
Smart positioning also leverages physics. Elevate your head and upper torso with an extra pillow, or slightly raise the head of the bed. Sleeping on your side may help if one nostril is more congested. During the day, gentle movement—short walks or light stretching—can promote circulation and reduce that heavy, “stuck” feeling without overexerting you.
Quick home routine for a congested evening:
– Rinse with isotonic saline, then rest for 10 minutes.
– Take a warm shower or inhale gentle steam for 5–10 minutes.
– Run a clean humidifier to 40–50% and elevate your head for sleep.
– Sip warm fluids; avoid smoky rooms and strong fragrances.
Making Sense of Over‑the‑Counter Relief: What Helps, What to Watch
Nonprescription options can be helpful when chosen thoughtfully and used correctly. Intranasal corticosteroid sprays reduce inflammation inside the nose, especially for allergy‑driven stuffiness. They work best with daily use and may take several days to reach full effect, so they are a solid option for ongoing symptoms rather than instant relief. Intranasal antihistamine sprays (where available) can calm sneezing and itching rapidly, with some benefit for congestion in allergic rhinitis.
Oral antihistamines are useful when histamine is the main culprit—think sneezing, itchy eyes, and clear watery drip from pollen or pet dander. Newer, less‑sedating options are often preferred for daytime use, while older sedating types may help at night but can impair alertness the next day. For purely viral congestion without allergy features, antihistamines usually do less for the “blocked” sensation.
Decongestants target swollen blood vessels. Oral forms containing pseudoephedrine can open passages but may raise blood pressure, speed heart rate, and disrupt sleep; they are not a fit for everyone, especially if you have hypertension, heart disease, thyroid issues, glaucoma, or prostate enlargement. Phenylephrine, another common oral ingredient, has limited evidence for meaningful nasal decongestion in many adults. Topical decongestant sprays act quickly and can feel dramatic, but limit use to no more than three days to avoid rebound congestion (rhinitis medicamentosa), which can turn a short‑term fix into a long‑term problem.
Supportive options include saline gels to moisturize dry linings and protect against cracking, and aromatic ointments with menthol or eucalyptus that can create a sensation of easier airflow—comforting, though they do not reduce swelling. Whatever you choose, read labels carefully and consider interactions with existing conditions or medications. If you are pregnant, have chronic illnesses, or are selecting options for a child, a conversation with a clinician or pharmacist is a wise pause before purchase.
How to choose wisely:
– Match the tool to the cause: steroids for allergy inflammation, decongestants for short bursts of swelling.
– Avoid topical decongestant sprays beyond three days.
– Consider daytime alertness and nighttime rest when selecting antihistamines.
– Check for blood pressure, heart, thyroid, glaucoma, or prostate cautions with decongestants.
Tuning Your Space and Daily Habits for Clearer Breathing
Your nose is a frontline filter, so what floats in your air matters as much as what you spray or swallow. Start with humidity: aim for 40–50% to keep mucus mobile and linings comfortable. Use a hygrometer to check levels, empty and dry humidifier reservoirs daily, and clean per manufacturer guidance to discourage mold and bacteria. Ventilate kitchens and bathrooms to reduce moisture buildup, and repair leaks promptly to prevent hidden damp spots that can fuel mold growth.
Allergen control can pay big dividends if your nose reacts to dust mites, dander, or pollen. Encase pillows and mattresses in allergen‑impermeable covers, wash bedding weekly in hot water (around 54°C/130°F), and vacuum with a HEPA‑equipped machine. During high pollen days, keep windows closed, change clothes after outdoor time, and shower before bed to avoid carrying allergens onto your pillow. Pet guardianship can coexist with clearer sinuses: keep pets out of the bedroom, use washable throws on favorite nap spots, and groom outdoors when possible.
Air quality also includes what not to breathe. Tobacco smoke, incense, and harsh cleaning fumes are common irritants that inflame nasal linings even in nonallergic noses. Choose fragrance‑free or unscented cleaners when practical, and crack windows briefly during and after cleaning to air out rooms—balanced with pollen considerations if that is a trigger for you. Portable air purifiers with HEPA filtration can help in bedrooms or living areas where you spend the most time; place them away from walls to improve airflow.
Daily habits round out the strategy. Gentle exercise encourages circulation and can ease the sense of pressure, while good hydration keeps secretions from turning gluey. Some people notice a brief “open” feeling after spicy foods due to a reflex runny nose; enjoy it if it helps, but it is a short‑term sensation rather than a treatment. Breathing through the nose during activity can train patterns that support humidification and filtration, while mouth breathing tends to dry the throat and may worsen morning stuffiness. Small, consistent environment and habit tweaks often stack into noticeably easier nights.
Room‑by‑room quick checks:
– Bedroom: 40–50% humidity, allergen‑proof covers, pet‑free sleeping zone.
– Bathroom: vented showers, dry towels, watch for mold at grout and caulk.
– Living room: HEPA vacuum routine, purifier placement, low‑fume cleaners.
– Entryway: shoe mat and coat area to keep outdoor pollen from spreading indoors.
When to Seek Medical Care and How to Prevent the Next Bout
Most congestion improves within a week or two with home measures and over‑the‑counter support. Still, some situations deserve prompt attention. Seek medical care if you have sinus pain and pressure with fever that lasts beyond a few days, symptoms persisting more than 10 days without improvement, severe one‑sided pain or swelling, repeated nosebleeds, vision changes, a severe headache with neck stiffness, wheezing or shortness of breath, or if you suspect a foreign body (especially in children). If you recently had a head injury and notice a persistent clear drip, get urgent evaluation. For infants who cannot feed well because of congestion, timely guidance is important.
Chronic patterns—symptoms lasting 12 weeks or recurring frequently—warrant a deeper look. Causes can include chronic rhinosinusitis, structural narrowing, nasal polyps, ongoing allergies, or irritant exposure at home or work. Clinicians may recommend targeted treatments such as prescription nasal sprays (including steroid, antihistamine, or anticholinergic options), short steroid tapers in select cases, allergy testing, or immunotherapy for well‑documented triggers. Imaging or a nasal exam may be suggested if structural issues are suspected. The goal is not only to calm the current flare but also to reduce future ones.
Prevention is a two‑lane road: fortify your defenses and reduce exposures. Wash hands regularly, especially during cold season; avoid touching your face; and keep shared surfaces clean. Stay up to date with recommended vaccines that lower the risk of respiratory infections. Manage indoor humidity, ventilate damp areas, and maintain allergen controls if those fit your history. When outdoor air quality drops—due to pollen spikes or smoke—limit exposure, close windows, and use filtration indoors. If heartburn or reflux worsens nighttime stuffiness, small changes like earlier dinners and head‑of‑bed elevation can help.
Bringing it all together: start with saline and steam, layer in humidity and smart positioning, and add pharmacy tools that match your pattern—steady anti‑inflammatory sprays for allergies, cautious short‑term decongestants for acute swelling. Tidy the air you live in, keep routines sustainable, and watch for the few warning signs that mean it is time to call a clinician. With that roadmap, most readers can trade the late‑night tissue scramble for steadier, quieter breathing—and a more restful tomorrow.